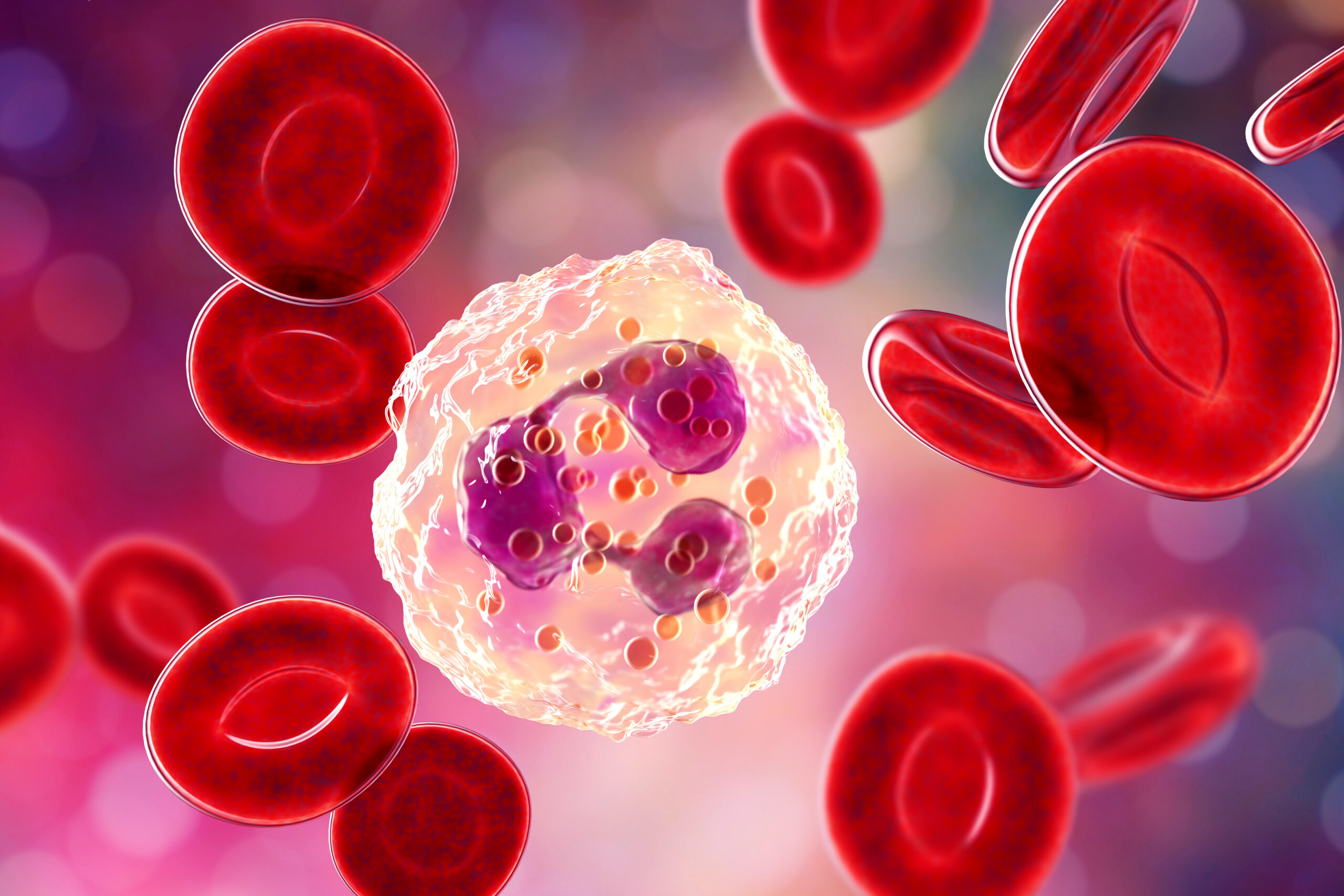
Neutrophils: First Responders, Fierce Defenders, and Key Targets in Disease
Neutrophils are the most abundant immune cell in human blood with around 1011 new cells synthesised in the bone marrow each day. These cells are short-lived, packed with anti-microbial proteins and are first responders upon inflammatory insult. Upon activation, neutrophils utilise effector functions to destroy pathogens.
Neutrophils release anti-microbial proteins held in granules in a process called degranulation and can phagocytose pathogens in as little as 20 seconds. They can also mount a large oxidative burst via the NADPH oxidase (NOX2) complex, releasing reactive oxygen species to kill extracellular pathogens, and also those that have been phagocytosed. The final weapon in the neutrophil arsenal is release of neutrophil extracellular traps (NETs) – web-like structures comprised of chromatin and antimicrobial proteins, released via a unique form of cell death called NETosis. These trap pathogens to prevent dissemination and expose them to high concentrations of antimicrobial proteins. Despite neutrophils being essential for host defence, dysregulated neutrophil responses can damage the host and drive inflammatory diseases, meaning targeting neutrophils could be of therapeutic benefit.
Neutrophils have been implicated in cancer progression and metastasis. For example, NETs have been shown to sequester circulating tumour cells and awaken dormant cancer cells, leading to metastases formation. Neutrophils can promote the premetastatic niche and neutrophil-deficient mice show reduced metastasis. They also drive Systemic lupus erythematosus (SLE) where NETs are a source of autoantigens and lead to vascular damage. SLE neutrophils also produce large amounts of type I interferons. Neutrophils have also been shown to play a detrimental role in atherosclerosis, where NETs aid in the formation of atherosclerotic plaques and prime macrophages to release pro-inflammatory cytokines. Overall, the role of neutrophils in disease is becoming increasingly understood and targeting these cells with therapeutics at the site of inflammation could benefit patients in many inflammatory diseases.
Burn, G. L., Foti, A., Marsman, G., Patel, D. F., & Zychlinsky, A. (2021). The Neutrophil. Immunity, 54(7), 1377–1391. https://doi.org/10.1016/j.immuni.2021.06.006
Papayannopoulos V. (2018). Neutrophil extracellular traps in immunity and disease. Nature reviews. Immunology, 18(2), 134–147. https://doi.org/10.1038/nri.2017.105 Coffelt, S. B., Wellenstein, M. D., & de Visser, K. E. (2016). Neutrophils in cancer: neutral no more. Nature reviews. Cancer, 16(7), 431–446. https://doi.org/10.1038/nrc.2016.52
Written by Will Gibbs



